Osteoporosis is a disease in which the bone becomes more porous, with more air inside, increasing the number and size of the cavities or cells that exist inside. In this way, the bones become more fragile, resist blows worse and break more easily. Fractures are indeed the symptom and the main consequence of this disease.
Osteoporosis does not cause symptoms until bone loss is so significant that fractures occur, and this usually occurs many years after menopause. There are, therefore, the following possible forms of onset and detection of the disease.
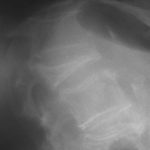
The fundamental test for the diagnosis of osteoporosis is Densitometry. Densitometry not only tells us about bone loss in a person. It can also document the response of the skeleton to an osteoporosis treatment. Plain x-rays of the bones are used to detect fractures.
In post-menopausal and elderly osteoporosis, laboratory analyzes are not usually altered. Calcium (blood and urine), phosphorus and protein levels are usually normal. Alkaline phosphatase is a substance in the blood that increases, in osteoporosis, when a fracture is being repaired, that is when the callus is forming. In some situations, it will be necessary to measure blood levels of vitamin D, thyroid hormones, or investigate kidney or liver function.
The aim of osteoporosis treatment is to reduce the number of fractures due to this disease. The fundamental tool to achieve this goal is to build a strong and resistant bone, and prevent its loss of bone mass. Although each person’s bone mass profile is conditioned by their genetic load, and this cannot be acted upon, it is important to raise awareness among the young population, especially females, that they ingest an adequate amount of calcium that they perform correct physical exercise and that they suppress harmful habits, such as alcohol and tobacco, in order to obtain a good amount of bone mass.